Light in the Darkness
02 Sep 2024
Personal stories and community efforts in the fight against Wilmington’s mental health crisis
Note: This article mentions suicide. If you or someone you know is having suicidal thoughts, call the Suicide & Crisis Lifeline at 9-8-8.
By Jade Neptune, founder of the Kinder Sea Foundation

At any given moment during my twelve-hour shift as a psychiatric technician, I could be anything: a priest, holding onto confessions like keepsakes as I read scripture from a pocket-sized Bible; an artist, shading inside the lines with broken crayons and dull colored pencils; a singer, stumbling off-key through the words of childhood lullabies; or a friend, making beaded bracelets and braiding hair. Most of the time, I’m an immeasurable mix of all the above. But in every moment, I am required, relentlessly, to be myself. I am a daughter, a sister, a friend, a student, a writer, and a founder. And I’m a mental health professional who struggles with her own mental illness.
The country is facing a growing mental and emotional crisis, and Wilmington is deeply affected, marked by chronic homelessness and opioid abuse. In 2023, nearly 600 people were documented as homeless in the Cape Fear region, and 11.6% of Wilmington’s adults engaged in opioid abuse, the highest rate in the U.S. Despite the urgent need for care, facilities are often understaffed and have limited beds. But these statistics don’t just affect faceless numbers—they affect real people.
The crisis touches every corner of our community, from the brave first responders who witness trauma every day, to the friends who struggle silently, to the children who are vulnerable in ways we might not always see. It could be your hero, your friend, your child. Their stories are not just tales of struggle, but of resilience, community, and the fight for mental health that we all must take part in.

Your Hero
To an extent, trauma is part of the job for any first responder, both experiencing it and helping community members through it. But this doesn’t make it easier. According to a study on First Responders’ Behavioral Health by the Substance Abuse and Mental Health Services Administration, 69% of EMS professionals have never had enough time to recover between traumatic events. First responders–including firefighters–are repeatedly put through harmful cycles, such as “repeated exposure to painful and provocative experiences and erratic sleep schedules.” The Wilmington Fire Department is no exception, but, like many departments, didn’t begin to discuss it openly until recently.
In WFD’s 2023-2026 Strategic Business Plan, one of the top concerns mentioned is that “Firefighters are not trained to handle issues for themselves or mental health emergencies in community.” At the time it was written, that was true.
“I was invincible,” says Lt. Josh Baltz. “Calls did not bother me. Not at all. I was like, ‘let's go.’ Craziest of the crazy, right? And then I went to a call involving a child. That destroyed me. I was a grown man crying with another grown man at our station… I never thought this would be me.”
For Lt. Baltz, the only services available to him when he sought support after his call was the department chaplain services. Then, he helped spearhead WFD’s Facility Dog program, a group of five (and counting) crisis response dogs at the station and on call to support firefighter mental health.
“In the world of firemen, we don't want to open up,” says Baltz. “We don't want to show weakness. We don't want to talk about our problems. The world now is definitely changing, and we've become a lot better with that. But even more so with this program, we're not coming out to say ‘hey, tell me what's going on, what happened?’ We're coming over, we're letting the dog do his thing.”
As if on cue, Baltz’ facility dog JETHRO, trained in partnership with PAWS for People™ and the larger WFD Mental Health and Wellness program, looked up at him from where he sat perched at his feet and snuggled into his boots.
“Year after year we've seen the calls for our team's activation increase,” he continues. “I wouldn't say that that's because there's more bad calls. I would say it's because more and more people are accepting the resource.”

Your friend
When I talk to my loved ones about my mental health, I usually receive a response along the lines of “you’re not alone.” I know this well because I work in an inpatient psychiatric facility where, for thirty six hours a week, often in a row, I run my fingers over the pebbled complexion of other peoples’ rock bottoms. Mental illness is like a waiting room: You’re never alone, and yet, that doesn’t make it easier. It’s one of the only places in the world where misery hates company.
This does not make me special. My brain grabs on to terrifying images and thoughts like sandspurs clinging to the vulnerable parts of your ankles. My breathing often comes in sharp spurts, like I’ve ran a marathon even though I’ve only had a conversation. A harsh blush climbs up my neck like a kudzu vine when I think too much and, sometimes, I’m afraid of the way I think. For the first eighteen years of my life, I was sure I was broken. For the last three, I’ve known that I have Obsessive-Compulsive Disorder, General Anxiety Disorder and Panic Disorder.
The longer I spend in the mental health field, the more arbitrary it feels for me to tell others about the way my brain tells me stories. I am a psychiatric technician, I am a graduate student studying clinical mental health counseling and will one day be a very proud, uniquely qualified counselor. And I am no different than my patients, or the faces I see on the streets as I drive home from work, or peers that I lost to suicide. None of us are.
I tell my story because I’ve been very lucky. I’ve been given an incredible gift to help others in my community who hurt the way I’ve hurt, who share the fears that I’ve had, and I have seen kindness work. But there is more to be done.

Your child
Anecdotally speaking, children are known to be beautifully, scientifically resilient. However, some are predisposed otherwise. A study form Harvard Pediatrics states, “the single most common factor for children who develop resilience is at least one stable and committed relationship with a supportive parent, caregiver, or other adult.” The same children who are less likely to be resilient are the same children who are more likely to develop mental health conditions, behavioral issues, and, in severe cases, criminal issues. According to NAMI, seven in 10 youth in the juvenile justice system have a mental health condition; one in six U.S. youth ages 6–17 experience a mental health disorder each year; and 128,000 North Carolinians ages 12–17 have depression.
At Novant Health, the behavioral health emergency department takes children as young as four. Many adolescents stay in the ED awaiting transfer to an inpatient facility, such as Carolina Dunes Behavioral Health in Leland or Old Vineyard Behavioral Health Services in Winston Salem. Some of these young patients could wait several months in the ED for long-term placement.
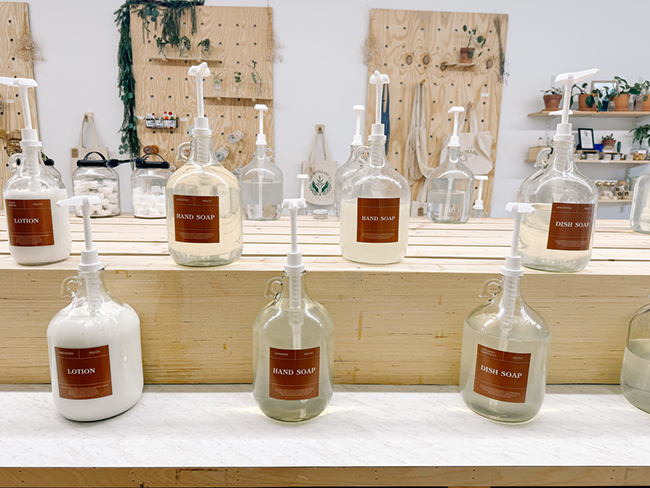
But from the ED to inpatient facilities, children often go without basic resources, where things like appropriate clothing, books, art supplies, and therapeutic fidget tools are scarce. Many young patients spend their time in hospital scrubs or in clothing that come in ripped, dirty, and, in some cases, soaking wet.
That’s where Kinder Sea Foundation found a need that we can all take part in filling. I started this nonprofit to uplift pediatric mental health in our community by offering resources, education and advocacy. By providing materials to local treatment facilities, offering youth mental health first aid training to community members, and raising awareness, we aim to connect clinical care to long-term healing.
Sometimes, the most therapeutic act you can offer a child in need is the things that make them feel like they’re in a childhood, rather than in crisis. For some, that means clothing or age-appropriate books; art supplies and notebooks for journaling; or academic materials that can support their journey to obtaining a GED or applying to college. Beginning this fall, we will begin donating these items to local pediatric facilities, hosting advocacy events. and providing Mental Health First Aid trainings.
Regardless of how I define myself on any given day, the most important thing I am for my patients is a human being who treats them like an equal. A person with a mental illness can be anyone, but so can an advocate. It could be you.
I hope you will join me in the fight against the ongoing mental health epidemic in our community, because you truly can make a difference.
Please stay tuned for more information on how to get involved at kindersea.org.