Protecting your Heart
30 Dec 2016
The New Hanover Regional Medical Center has a new program to help congestive heart failure patients live with their disease
By JESSICA SMITH
As many Wilmington residents know, the Heart Center at New Hanover Regional Medical Center (NHRMC) offers a wide array of heart screenings and diagnostic tests to determine patients’ general heart health. The Center’s surgeons and cardiologists are well-qualified to treat every heart disease from angina to peripheral arterial disease.
Now there’s good news for local residents suffering from congestive heart failure, a serious medical condition in which the heart cannot pump enough blood to meet the body's needs.
In 2014, the Heart Center expanded its services with the addition of the Congestive Heart Failure Program, which provides treatment for those diagnosed with heart failure. Within 18 months, NHRMC hired Dr. John Rommel, a cardiologist with the Cape Fear Heart Associates practice, to lead the program and extend its reach. The team currently includes four nurse practitioners, one heart center nurse and a pharmacist in addition to Dr. Rommel.
Patients enter the program after a referral from another cardiologist or from their primary care physician. Occasionally, patients seeing other specialists in the hospital come in for a consultation, and from that point on the program stays actively involved with their care.
While people generally show signs of heart failure for some time before they seek medical attention, many of the signs are not heart-specific – and are easily overlooked. “Patients will notice swelling in their legs, a feeling of general fatigue or a persistent cough, but they often attribute these symptoms to a virus or a cold,” explains Dr. Rommel.
Other patients enter the program after an acute episode, such as a heart attack or the sudden onset of heart failure. The program makes sure that every patient is receiving the best in evidence-based care, offering a variety of ACE inhibitors, beta blockers and diuretics to relax blood vessels, reduce blood pressure and regulate fluid in the body.
“We experiment to offer our patients the highest dose of evidence-based medications that they can tolerate. We help them make lifestyle modifications, and watch carefully to see if they’re improving,” said Dr. Rommel.
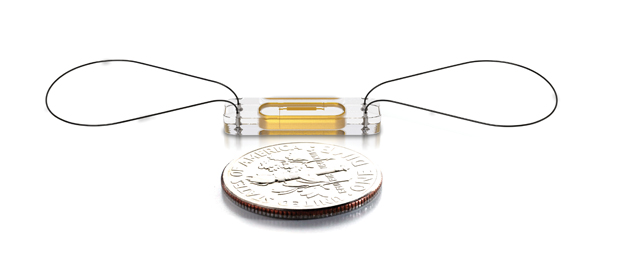
To help with patient surveillance, the program has recently begun piloting a new remote device called CardioMEMS™, an FDA-approved monitoring system that detects signs of worsening heart failure. “This dime-sized device is implanted in a patient’s pulmonary artery,” explains Dr. Rommel. “It senses any changes in the pulmonary artery pressure and heart rate, and emits a frequency to convey that information wirelessly.”
The device is permanently placed in the patient’s pulmonary artery, the blood vessel that moves blood from the heart to the lungs, during a one-day outpatient procedure. Afterwards, the patient takes a daily reading from the device by lying down on a specialized pillow equipped with an antenna. The antenna picks up the signals emitted from the device, interprets the data and releases that information to the internet, where staff from the program can access it.
“If a patient’s pressure is rising or their fluid levels are building up, we can step in and give them diuretics in order to keep them out of the hospital,” says Bridget Williams, nurse practitioner with Cape Fear Heart Associates and the Congestive Heart Failure Program. “A lot of heart failure centers around the country are focusing on monitoring devices like this, because they allow us to better manage our patients beyond a weekly hospital visit or calls to check in and see how they’re doing.”
The program also offers a four-week series of classes for patients enrolled at the Heart Clinic. Run by the pharmacist and student volunteers, the classes cover topics as diverse as the disease process, lifestyle modifications and how to establish end-of-life care goals. A nutritionist also participates, offering expert advice on how the patient can effectively make changes to his or her diet.
In the last few years, several new drugs have also come on the market to help prolong life expectancy in heart failure patients. “Our pharmacists are a huge part of the process for us,” says Williams. “We’re getting our patients switched over to the most effective medicines so that they can get exactly what they need.”
For those who are really struggling, the program considers IV medication, which provides medicines through a pump. “If necessary, we reach out to the advance therapy centers in the area to see if they are candidates for transplants,” says Dr. Rommel. Surgical options for heart failure include coronary artery repair, valve repair or replacement, implantable cardiac defibrillators, biventricular pacemakers and heart transplants.
While the program does not yet perform these surgeries, it partners extensively with hospitals such as UNC Health Care in Chapel Hill or Duke University in Durham, which provide heart transplants and device placement.
“Our program provides heart failure patients in the larger Wilmington area with local services, so they don’t have to drive three hours to see a doctor,” says Dr. Rommel. “It also provides reassurance to the centers doing these advanced therapies. Knowing that there are specialists in Wilmington who can help manage transplants postoperatively helps when they evaluate whether or not a local patient is a good candidate for surgery.”
For patients who have already had a heart transplant or a left ventricular device, the program works to manage their health care needs after they come home from the hospital. The program’s staff remains active in making sure that patients are completing the appropriate medical therapy.
“Our main goal is to help our patients stay feeling better, and keep them relatively healthy in the context of their heart failure,” said Dr. Rommel.
Staying Heart-Healthy
For those without heart problems who are looking for tips on becoming heart-healthy, the most important advice is simply to get up and move. “A lot of people tell you they can’t find the time to exercise for 30 minutes a day, but everyone can certainly do five minutes a day,” says Williams. “People need to get up and move as much as possible.”
Challenge yourself to an achievable daily goal, such as ten minutes of moderate activity. Then continuously up your goal every month until you’re achieving what you want to achieve – and you’ve cemented your good habits. Recent studies indicate that it takes far longer than was previously thought to get accustomed to a new behavior. If you really want your lifestyle changes to stick, you need to keep at them for at least two months on average before your changes become automatic.
“Fortunately and unfortunately, there’s no easy trick – but there are several things that you can do that will really work,” says Dr. Rommel. “The simple advice you always hear is the only advice for us all: Watch what you eat, watch your diet and try to stay active every day.”
Limit Your Salt
Limiting your salt consumption can also make a huge difference in your heart health. The average American eats more than 3,400 milligrams (mgs) of sodium per day, which is far more than the upper limit of 2,300 mgs recommended by the American Heart Association (AHA). Ideally, the AHA recommends no more than 1,500 mg per day, but food labels are still based upon the higher number.
For those with high blood pressure or heart disease, the recommendation is of critical importance. Extra sodium in the bloodstream pulls water into your blood vessels, increasing the volume of blood. In turn, this increases your blood pressure as the heart works overtime to adjust to the force needed to pump blood through the body. High blood pressure tires your heart prematurely and contributes to the deterioration of your vessels.
In the Congestive Heart Failure Program, the staff urges patients to commit to consuming no more than 2,000 grams of salt a day. “We show them the actual sodium content from their favorite fast food places,” says Williams. “You can find the nutrition information for almost every restaurant online. It’s important to know exactly what you’re eating.”
Packaged or pre-made food is usually laden with extra sodium. In fact, only about 12% of the sodium you eat occurs naturally in your food; more than 75% of the sodium in our diets is added during processing. A single-patty fast food hamburger averages 378 milligrams of sodium — and that’s before ketchup and other condiments. With all the fixings, that burger averages around 1,000 milligrams of sodium, or 66% of your ideal daily limit.
If you’re a parent, try to limit your children’s salt intake as well. Factors that contribute to high blood pressure, heart disease and stroke begin in childhood, and studies show that a high sodium intake can also increase the risk for kidney disease, osteoporosis and stomach cancer.
As Williams says, “Push yourself away from the table, and leave the salt shakers alone!”
Eat More Fruits and Vegetables
Although those of us who grew up with the food pyramid should know better, the truth is that very few Americans actually eat the three to five servings of vegetables and two to four servings of fruit recommended by the U.S. Department of Health and Human Services. In fact, the Centers for Disease Control and Prevention (CDC) has reported that only 33% of adults eat the daily recommended amount of fruit, and only 27% eat as many vegetables as they should.
If you want to improve your heart health, however, this is by far the simplest way to start. Fruits and vegetables are naturally low in fat, sodium and calories, and they have no cholesterol. They are also high in fiber and are often brimming with antioxidants that can help you maintain a healthy heart.
Consider exploring some of the so-called superfoods for your heart. Non-processed oatmeal, chia seeds and soy milk help to reduce cholesterol, while raisins can help to lower blood pressure and control hypertension. Blueberries, broccoli and cauliflower are full of antioxidants that help to protect your heart, and brussels sprouts can even help control inflammation in your cardiovascular system.
Get a Physical
The team at NHRMC agrees that getting a general physical once a year is an important screening measure for heart disease. Be honest with your doctor, and take a good hard look at your results to determine if any lifestyle modifications are needed. In addition to a complete blood count, chemistry panel, urinalysis and blood sugar check, a lipid panel to test your cholesterol levels is recommended every four years.
Also known as a lipid profile, this simple blood test requires that you fast overnight before having your blood drawn. Your results will show you your total cholesterol levels, and will determine whether your low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol levels fall within the acceptable ranges.
Above all, stay alert about how you’re feeling. You are your own best witness. “Be cognizant of any changes happening in your body, and don’t dismiss them,” reminds Dr. Rommel. “People are usually showing signs or symptoms of heart failure before they start to look.”